Intervju med Murali
Om professor Schallreuter's behandling som har bidragit till att minska hans vitiligo.
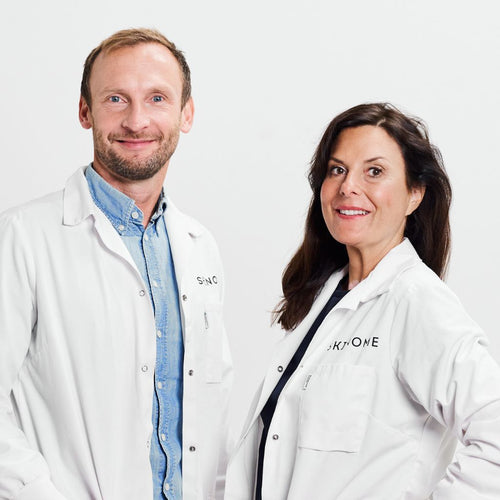
Intervju med Skinome's grundare Johanna Gillbro, om hennes upplevelse med PC-KUS behandlingen
Jag har haft vitiligo sedan min barndom. Jag besökte många hudläkare och provade allt från kortison, takrolimus och UVB-behandling till transplantation av friska pigmenterade hudceller till de drabbade områdena. Inget fungerade och vitiligon blev faktiskt värre av alla behandlingar.
Jag studerade i Uppsala till farmaceut och tog examen 2002. Under mina år på universitetet fick jag kontakt med den tyska hudläkaren och hudforskaren Karin Schallreuter som var professor vid University of Bradford och expert på vitiligo (se video klipp). Denna kontakt gav mig möjlighet att genomföra doktorandstudier i klinisk och experimentell dermatologi med Schallreuters team.
Baserat på upptäckten av ”fjärilsbioterinerna” i vitiligofläckarna utvecklade Karin Schallreuter och hennes team en behandling för att minska oxidativ stress i huden. När behandlingen användes bleknade melanocyterna och började producera pigment igen. Idag använder jag NB-UVB-aktiverat pseudocatalase PC-KUS med mycket bra effekt, mitt ansikte och ben har fått 90% repigmentering. Händer och fötter är dock fortfarande svåra att behandla.
Denna behandling utvecklades av professor Schallreuter 1995 och har sedan dess hjälpt tusentals patienter på tre olika platser: Medical Clinic-The Dead Sea, Institute for Pigmentation Disorders av V. Greifswald, Tyskland och vid University of Bradford, England. 2006 försvarade jag min avhandling om vitiligo och tog en doktorsexamen i experimentell dermatologi. Idag känner jag mig glad över min vitiligo och njuter av de vita fläckarna, även om flera av dem nu helt försvunnit. Om jag inte hade haft dem hade jag förmodligen inte haft den motivation jag har, inte heller hade jag upplevt allt jag har upplevt eller träffat alla dessa fantastiska människor och forskare som jag mött genom åren.
Om du är intresserad, läs gärna de vetenskapliga publikationerna om behandlingen här.
/Johanna Gillbro